Conditions
At RPSA, we take pride in offering comprehensive diagnosis and treatment options for a wide range of complex gynecological conditions. We understand how important it is for our patients to feel heard and understood, which is why we take a patient-centered approach. We believe in providing our patients with personalized care tailored specifically to their unique needs and circumstances. Our team, led by Dr. Iskander, has a deep commitment to advocating for each patient and helping them understand their diagnosis and treatment options. We strive to empower our patients to make informed decisions about their care and work closely with them to develop optimal treatment plans that meet their individual goals. Whether you’re dealing with a challenging condition or simply seeking routine gynecological care, we are here to support you every step of the way.
Fibroids are non-cancerous growths consisting of muscle and fibrous tissue located inside the uterus and varying in size.
Symptoms of uterine fibroids
Fibroids in the uterus do not always have symptoms. However, common symptoms of uterine fibroids may include:
- Heavy menstrual bleeding, sometimes with the passage of blood clots
- Longer than normal menstrual periods
- Pelvic cramping or pain during periods
- Bleeding between periods
- Sensation of fullness or pressure in the lower abdomen
- Need to urinate more frequently
- Pain during sex
Fibroids can develop anywhere in the uterus, and more than one may develop over time. Large fibroids that distort the shape of the uterus or uterine cavity most frequently affect fertility, prohibiting an embryo from implanting
Fibroids are quite common in people of reproductive age, affecting 85% of women. Most Fibroids usually go undetected and cause no symptoms, though Fibroids can cause various symptoms, including abnormal vaginal bleeding and abdominal and pelvic pain….
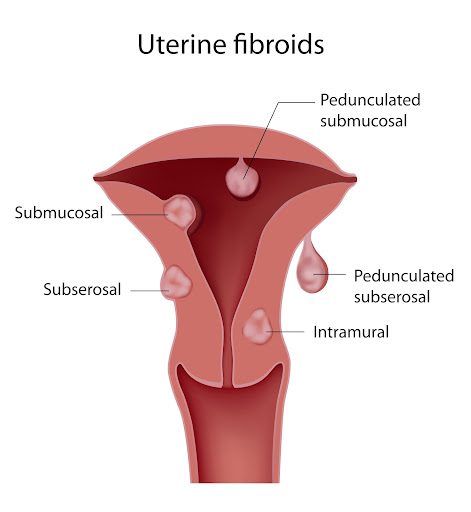
Fibroids are named depending on their location:
- Subserous Fibroids: Grow in the muscle of the uterus, expanding outside the uterus into the pelvic area
- Intramural Fibroids: Grow within the muscle of the uterus
- Submucosal Fibroids: Grow towards the inner wall and expand in the endometrial cavity
Generally speaking, Fibroids, no matter their type, grow slowly. However, among many factors, high levels of Estrogen can make these Fibroids grow faster.
Typically, Fibroids are benign tumors. They could, although rarely, become cancerous, with this only happening between 1 in 500 and 1 in 2000 people.
As mentioned, most people with Uterine Fibroids experience no symptoms. However, 1 in 3 people with Fibroids experience symptoms, mostly related to the size and the location of the Fibroids.
These symptoms include:
- Heavy bleeding during periods with blood clots and cramps
- Abdominal or lower back pain
- Frequent need to urinate
- Constipation
- Deep pain during sex
- Infertility or difficulty conceiving
Any person of reproductive age can get Fibroids from puberty to menopause. Because their growth is related to the hormone Estrogen, Fibroids can potentially shrink away after the onset of Menopause.
To diagnose Fibroids, your doctor will ask for a medical history and a pelvic exam. Large Fibroids can be detected through vaginal or abdominal examinations.
Tests to detect Fibroids may include:
- Blood tests to detect anemia associated with heavy periods, a symptom of Fibroids
- Ultrasound
- MRI.
Treating your Fibroids will depend on the symptoms associated with this condition. It also depends on their size, location, and future fertility plans.
Most of the time, Fibroids can be left untouched and just monitored. You may be prescribed medication to treat symptoms of pain or heavy periods. Other times, Fibroids might need to be surgically removed. Based on your evaluation, this is a shared decision you can make with your doctor.
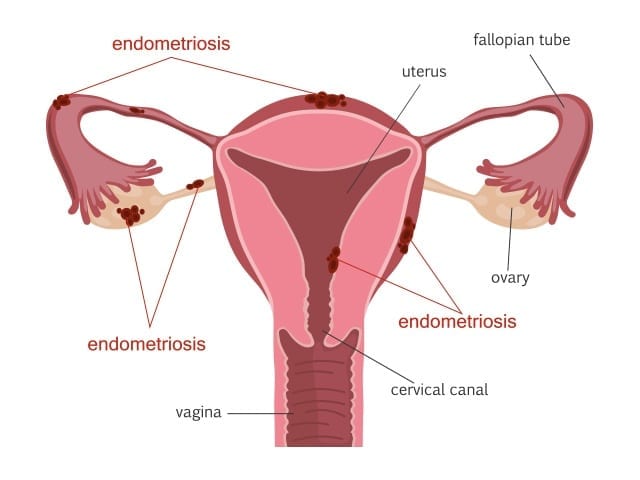
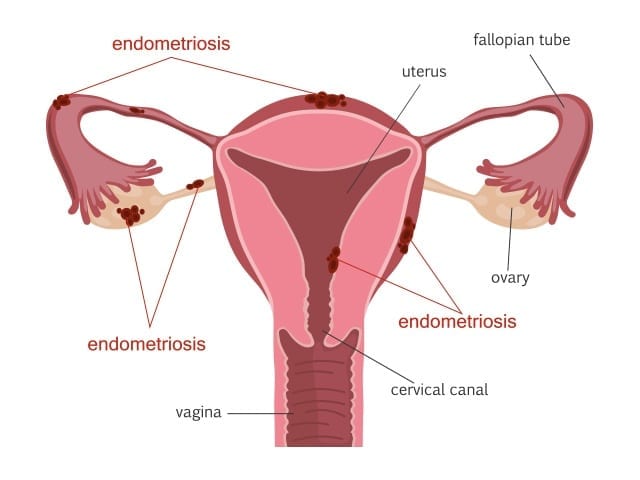
Endometriosis is defined by the presence of endometrial-like tissue outside the uterus.
Endometriosis affects the lining of the pelvis (peritoneum), the fallopian tubes, the ovaries, and the uterus. It could also affect other pelvic structures like the bladder, the bowels, and the pelvic nerves, and could grow outside the pelvis, affecting the lungs, diaphragm, etc……
1 in every ten women is affected with Endometriosis during their reproductive years. Although it is a common condition, it is sometimes misdiagnosed or mistreated, taking up to 7 years from the onset of pain to diagnosis.
Multiple risk factors for Endometriosis have been identified; however, this information must be treated carefully and with caution, as knowledge about the causes and development of Endometriosis is not yet definite. Research is still ongoing to determine what the causes may be.
These risk factors may include:
- Family history of Endometriosis
- Never having given birth
- Short periods
- Heavy and long periods
- Low BMI
- History of high estrogen production
- Late menopause
- Early onset of a period
- Reproductive system irregularities
Although sometimes people with Endometriosis can be asymptomatic, many people do experience painful and uncomfortable symptoms, such as:
- Painful periods
- Pelvic pain throughout the cycle
- Intestinal pain
- Fatigue and unease
- Painful sex
- Difficulty conceiving and infertility
- Painful urination or bowel movements
- Blood in urine or bowel near the time of menstruation
- Pain radiating into the back, down the legs, and sometimes into the chest
- Shoulder and neck pain
- Fatigue
- Dizziness with cycle
- Recurring constipation/diarrhea
To identify and diagnose Endometriosis, we can perform the following examinations:
- Pelvic examination
- Ultrasound
- MRI
- Laparoscopy
Endometriosis can be classified into stages:
- Stage One: Minimal Endometriosis
Characterized by minimal superficial lesions and no significant adhesions
- Stage Two: Mild Endometriosis
Characterized by superficial and deep lesions with no significant adhesions
- Stage Three: Moderate Endometriosis
Characterized by multiple deep lesions, small cysts on ovaries, and translucent adhesions
- Stage Four: Severe Endometriosis
Characterized by severe and multiple deep lesions, large cysts on ovaries, and dark adhesions.
These stages are based on the location, adhesions, spread, and depth of the Endometriosis and will be determined by your doctor upon examination.
If you have been diagnosed with Endometriosis, different treatment options depend on the stage, symptoms, and condition. For some people, this disease is manageable, while for others, it is debilitating and causes disruption of daily life and routines.
Treatment can include painkillers for mild conditions or a minimally invasive surgical excision of Endometriosis.
Endometriosis excision is when the endometriotic lesions are removed surgically while preserving the uterus, fallopian tubes, and ovaries. This minimally invasive surgery is the most effective treatment for Endometriosis and should only be done by trained specialists.
People with severe deep infiltrating Endometriosis benefit highly from excision surgery. The improvement after this procedure for people with such cases is usually striking and highly successful.
Other treatments for Endometriosis include:
- Pelvic floor physiotherapy
- Pelvic floor Botox
- Change in diet
- Acupuncture
- Assessing and avoiding environmental triggers
Isthmocele or C-section scar defect or Uterine Niche
An isthmocele is an indentation or discontinuation in the uterine wall that results in the location of a Cesarean section scar. Its causes aren’t completely understood, but it is thought to be related to incomplete or abnormal healing of the uterine incision. This scar defect weakens and thins out the uterine wall at its location.
Isthmoceles can be asymptomatic but may produce symptoms and complications such as:
- Postmenstrual spotting,
- Painful periods,
- Painful intercourse
- Chronic pelvic pain
- Possible infertility
- Risk of uterine rupture or placental adhesion during pregnancy

Diagnosis
A uterine isthmocele can be detected incidentally on ultrasound or purposefully looked for by the physician if a patient is symptomatic.
The most accurate way to diagnose an isthmocele is with a saline infusion sonohysterogram (SIS). During this procedure, your gynecologist will inject a small amount of sterile saline into the uterine cavity through the vagina and visualize the lining using an ultrasound.
MRI is also used for the diagnosis of isthmocele.
Treatment
There are several ways in which a uterine niche could be treated ranging from expectant management and pharmacological treatment to surgery. Surgery could be done through open, minimally invasive, hysteroscopic and vaginal approaches. Hysteroscopy and laparoscopy are the most common approaches and desire for future fertility plays an important role in choosing a treatment modality.
- Hysteroscopy: Your doctor would shave or cauterize the defect from the inside. This works best for women with abnormal bleeding, a thick wall and no desire for future pregnancy.
- Laparoscopic repair: Your gynecologist would completely remove the defect and reconstruct the wall of the uterus. This option allows for a healthy future pregnancy as it removes the frail part of the muscle.
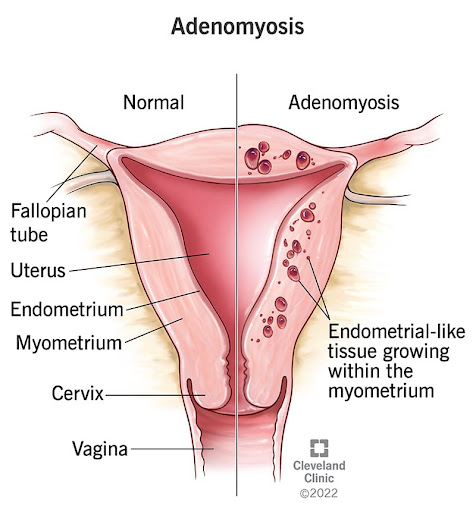
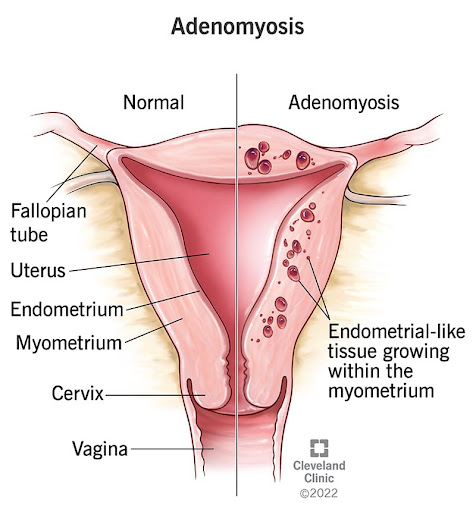
Adenomyosis is when tissue that lines your uterus grows into the muscular walls of your uterus.
It is ‘the presence of endometrial glands and stroma within the uterus or myometrium muscle. During monthly menstruation, this embedded tissue bleeds, leading to intense pelvic pain, inflammation and swelling, and heavy bleeding.
This condition is often misunderstood or misdiagnosed as Adenomyosis, often called Endometriosis of the uterus muscle, which causes both painful and heavy periods, painful sex, or dyspareunia.
With Endometriosis, spots of endometrial lining are located outside of the uterus, while in the case of Adenomyosis, this tissue is inside the muscle of the uterus… or an “Inside-Out Endometriosis”, as it used to be known.
To date, Adenomyosis has no clear causes, which can be frustrating. Studies have shown that people who have given multiple births and already suffer from Endometriosis are more at risk for Adenomyosis.
To diagnose Adenomyosis, a doctor will examine you and assess your symptoms. With this condition, the uterus may feel big, soft, tender, and sensitive to the touch.
Tests that your doctor can perform are:
- Ultrasound
- MRI
- Pathology examination after a Hysterectomy procedure.
As far as treatment goes, the symptoms of Adenomyosis can be dealt with by taking pain medication or by preventing monthly menstruation with hormonal treatment:
- Pain medication: The pain associated with Adenomyosis can be debilitating. Analgesics, anti-inflammatories, or strong painkillers can be prescribed.
- Hormonal Treatment: This is not a cure, as the pain will return if the treatment is stopped. Oral contraceptive pills, contraceptive implants (hormonal IUD), or injections can be suggested by your doctor to relieve pain and stop monthly periods.
- Surgery: If Adenomyosis is localized, it could be surgically excised. Sometimes the only solution to Adenomyosis is to remove the entire uterus. This procedure is called a Hysterectomy and may be suggested by your doctor based on your medical history, the extent of pain, and other symptoms.
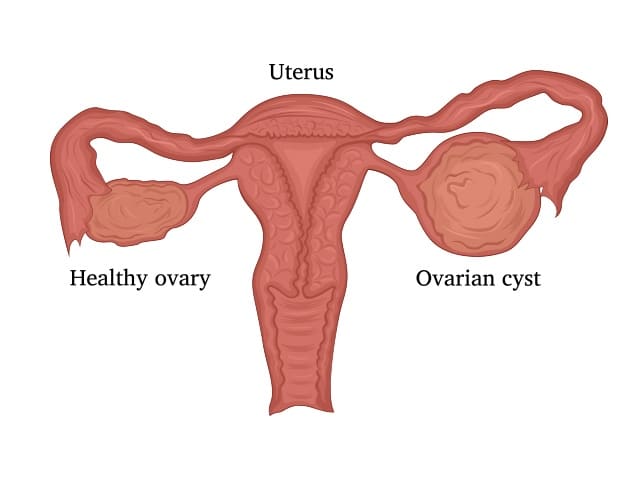
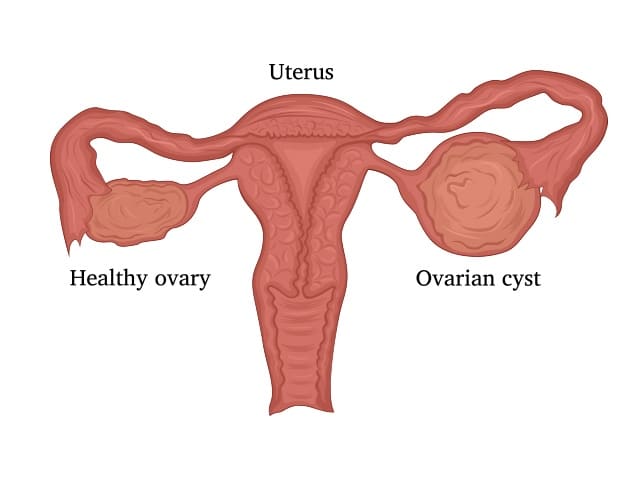
Ovarian Cysts are growths developing within the ovaries
Most Ovarian Cysts are harmless and are not cancerous. Cysts on the ovaries can sometimes grow as big as a watermelon, whereas a normal ovary is around the size of an almond.
Ovarian Cysts are most common before Menopause, occurring in around 7% of women.
Although Ovarian Cysts are not necessarily harmful or cancerous, they should be taken seriously, because they could indicate other underlying conditions. Identifying and examining Ovarian Cysts is necessary to rule out cancer and any underlying causes, such as Endometriosis.
Ovarian Cysts can come in many different forms, each with a different cause:
- Functional cyst: These cysts form because of normal function of the ovaries. When ovulation does not happen and a follicular cyst remains in the ovaries, and the opening where the egg escapes is closed off with accumulated fluid.
- Pathological cyst: These cysts form because of disease, but are not necessarily cancerous.
- Dermoid cysts: These cysts grow with the existence of developmental tissue that can contain teeth, bone, or hair.
- Hemorrhagic cysts: These cysts form due to bleeding.
- Endometriomas: These cysts are caused by Endometriosis, and are a sign of a severe form of the condition, accompanied with a lot of pain.
- Cancerous cysts: These cysts are rare, but commonly affect post-menopausal people, with vague symptoms that can go undiagnosed.
With Ovarian Cysts, most symptoms are not always noticeable. With Endometriomas, however, the main symptom is severe pain, even when the cysts are small.
If the cysts are large, regardless of their type, symptoms can include pain and swelling in the abdominal area. Cysts can also lead to constipation or frequent urination due to the cysts pressing on other organs in the abdomen.
Complications of Ovarian Cysts can include twisting of the ovary, bleeding, or bursting of cysts, which can cause severe pain and bleeding, usually requiring emergency attention and treatment.
Diagnosing Ovarian Cysts can be done by assessing medical history and by examination. These tests include:
- Ultrasound
- Blood tests
- MRI
- CT scan
Your doctor should monitor some cysts, while others don’t need monitoring at all. Functional Cysts may go away on their own without being treated.
Some cysts require surgery, and this should be determined by your doctor, depending on the Condition
AUB, Abnormal Uterine Bleeding
AUB, Abnormal Uterine Bleeding, sometimes referred to as Abnormal Vaginal Bleeding, is a term used to refer to heavy periods or bleeding between normal periods. It is a common condition affecting around 10% to 20% of women in the US.
Menorrhagia, also known as heavy periods, occurs when excessive blood is lost during monthly menstrual cycles.
Metrorrhagia, also known as bleeding between periods, occurs when uterine bleeding occurs between menstruations.
AUB is not just uncomfortable and inconvenient, but it can also affect the person’s quality of life, whether physical, mental, or emotional.
This condition is not always associated with physical abnormalities. Approximately 40% to 60% of people with heavy periods have no specific underlying cause.
AUB is associated with:
- Leaking through sanitary pads
- The necessity for double protection
- Flooding of menstrual blood onto clothes
- Large clots in the blood
- Sensations of weakness, tiredness
- Anemia
- Planning daily life around menstruation
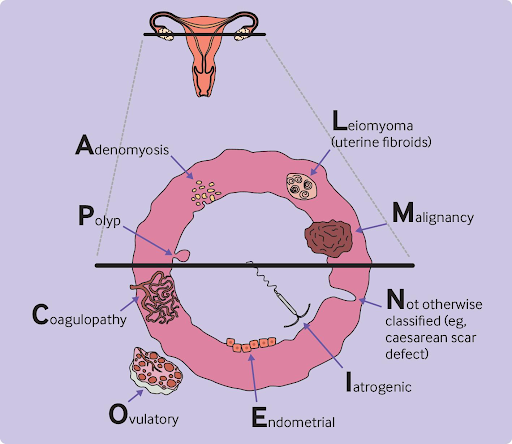
Although the majority of people with AUB have no specific underlying cause, there are some known reasons :
- Polyps: non-cancerous growths in the lining of the uterus
- Endometriosis: when developed in the vagina and/or the lower uterus
- Fibroids: benign growths on the walls of the uterus
- Adenomyosis: when glands from the uterus lining embed in the muscle of the uterus
- Cancer: uterine cancer is uncommon but can cause heavy periods
- Thyroid disease: thyroid disease can cause tiredness, weight gain, changes in hair and skin, intolerance to colds, and AUB
- Clotting problems: platelet problems or certain diseases can affect clotting and increase AUB
- Medical treatments: some medical treatments, such as hormonal contraceptives, anticoagulants, and anti-cancer drugs, can cause AUB
- Blood tests,
- Ultrasound
- Hysteroscopy (a camera to visualize the cavity of the uterus)
As for treatments, there are many options available, including:
- Hormonal and non-hormonal treatments
- Endometrial ablation
- Minimally invasive surgical removal of fibroids and polyps
- Hysterectomy
Tubo-ovarian abscess
A tubo-ovarian abscess (TOA) is an infectious mass found in the fallopian tube, ovary, or near those structures. It can be due to several factors that introduce an infection, but it usually develops as a pelvic inflammatory disease (PID) complication. PID is an infection of the pelvic reproductive organs that results mainly from untreated sexually transmitted infections.
Bacteria can travel up the vagina into the uterus, reaching the tubes and ovaries to form a walled-off cyst known as a tubo-ovarian abscess. TOAs occur in around 15% of patients with PID and are usually polymicrobial, meaning several types of bacteria are isolated from the abscess.
A TOA can be life-threatening should it rupture and cause sepsis, a widespread infection in the patient’s bloodstream.
Risk factors for developing a TOA include:
- Young age
- Multiple sexual partners
- Sexually transmitted infections
- Uterine instrumentation, such as insertion of an IUD with an active infection or a dilation and curettage (D&C)
- Hysteroscopy

Symptoms
- Lower abdominal pain
- Fever and/or chills
- Vaginal discharge
- Painful intercourse
- Nausea & vomiting
Evaluation & Diagnosis
On suspicion of a tubo-ovarian abscess, your doctor will perform a transvaginal ultrasound and may be able to identify the mass. Further imaging, usually a CT scan, might be needed to visualize the abscess better.
Although not commonly used, laparoscopy is still considered the definitive diagnostic tool and may allow for drainage and culture of the abscess.
Treatment
The first step in managing a TOA is starting antibiotics to avoid a widespread infection. Imaging-guided drainage by a radiologist could be attempted during antibiotic treatment.
While on this regimen, patients should be monitored for worsening symptoms or lack of improvement, which would then require surgical intervention to remove the abscess along with the affected tube or ovary.
Complications
- Recurrent PIDs
- Chronic pelvic pain
- Ectopic pregnancy, outside of the uterus
- Infertility
Fibroids are non-cancerous growths consisting of muscle and fibrous tissue located inside the uterus and varying in size.
Symptoms of uterine fibroids
Fibroids in the uterus do not always have symptoms. However, common symptoms of uterine fibroids may include:
- Heavy menstrual bleeding, sometimes with the passage of blood clots
- Longer than normal menstrual periods
- Pelvic cramping or pain during periods
- Bleeding between periods
- Sensation of fullness or pressure in the lower abdomen
- Need to urinate more frequently
- Pain during sex
Fibroids can develop anywhere in the uterus, and more than one may develop over time. Large fibroids that distort the shape of the uterus or uterine cavity most frequently affect fertility, prohibiting an embryo from implanting
Fibroids are quite common in people of reproductive age, affecting 85% of women. Most Fibroids usually go undetected and cause no symptoms, though Fibroids can cause various symptoms, including abnormal vaginal bleeding and abdominal and pelvic pain….
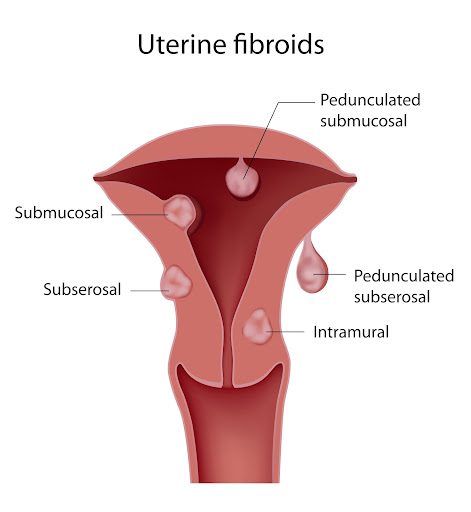
Fibroids are named depending on their location:
- Subserous Fibroids: Grow in the muscle of the uterus, expanding outside the uterus into the pelvic area
- Intramural Fibroids: Grow within the muscle of the uterus
- Submucosal Fibroids: Grow towards the inner wall and expand in the endometrial cavity
Generally speaking, Fibroids, no matter their type, grow slowly. However, among many factors, high levels of Estrogen can make these Fibroids grow faster.
Typically, Fibroids are benign tumors. They could, although rarely, become cancerous, with this only happening between 1 in 500 and 1 in 2000 people.
As mentioned, most people with Uterine Fibroids experience no symptoms. However, 1 in 3 people with Fibroids experience symptoms, mostly related to the size and the location of the Fibroids.
These symptoms include:
- Heavy bleeding during periods with blood clots and cramps
- Abdominal or lower back pain
- Frequent need to urinate
- Constipation
- Deep pain during sex
- Infertility or difficulty conceiving
Any person of reproductive age can get Fibroids from puberty to menopause. Because their growth is related to the hormone Estrogen, Fibroids can potentially shrink away after the onset of Menopause.
To diagnose Fibroids, your doctor will ask for a medical history and a pelvic exam. Large Fibroids can be detected through vaginal or abdominal examinations.
Tests to detect Fibroids may include:
- Blood tests to detect anemia associated with heavy periods, a symptom of Fibroids
- Ultrasound
- MRI.
Treating your Fibroids will depend on the symptoms associated with this condition. It also depends on their size, location, and future fertility plans.
Most of the time, Fibroids can be left untouched and just monitored. You may be prescribed medication to treat symptoms of pain or heavy periods. Other times, Fibroids might need to be surgically removed. Based on your evaluation, this is a shared decision you can make with your doctor.
Endometriosis is defined by the presence of endometrial-like tissue outside the uterus.
Endometriosis affects the lining of the pelvis (peritoneum), the fallopian tubes, the ovaries, and the uterus. It could also affect other pelvic structures like the bladder, the bowels, and the pelvic nerves, and could grow outside the pelvis, affecting the lungs, diaphragm, etc……
1 in every ten women is affected with Endometriosis during their reproductive years. Although it is a common condition, it is sometimes misdiagnosed or mistreated, taking up to 7 years from the onset of pain to diagnosis.
Multiple risk factors for Endometriosis have been identified; however, this information must be treated carefully and with caution, as knowledge about the causes and development of Endometriosis is not yet definite. Research is still ongoing to determine what the causes may be.
These risk factors may include:
- Family history of Endometriosis
- Never having given birth
- Short periods
- Heavy and long periods
- Low BMI
- History of high estrogen production
- Late menopause
- Early onset of a period
- Reproductive system irregularities
Although sometimes people with Endometriosis can be asymptomatic, many people do experience painful and uncomfortable symptoms, such as:
- Painful periods
- Pelvic pain throughout the cycle
- Intestinal pain
- Fatigue and unease
- Painful sex
- Difficulty conceiving and infertility
- Painful urination or bowel movements
- Blood in urine or bowel near the time of menstruation
- Pain radiating into the back, down the legs, and sometimes into the chest
- Shoulder and neck pain
- Fatigue
- Dizziness with cycle
- Recurring constipation/diarrhea
To identify and diagnose Endometriosis, we can perform the following examinations:
- Pelvic examination
- Ultrasound
- MRI
- Laparoscopy
Endometriosis can be classified into stages:
- Stage One: Minimal Endometriosis
Characterized by minimal superficial lesions and no significant adhesions
- Stage Two: Mild Endometriosis
Characterized by superficial and deep lesions with no significant adhesions
- Stage Three: Moderate Endometriosis
Characterized by multiple deep lesions, small cysts on ovaries, and translucent adhesions
- Stage Four: Severe Endometriosis
Characterized by severe and multiple deep lesions, large cysts on ovaries, and dark adhesions.
These stages are based on the location, adhesions, spread, and depth of the Endometriosis and will be determined by your doctor upon examination.
If you have been diagnosed with Endometriosis, different treatment options depend on the stage, symptoms, and condition. For some people, this disease is manageable, while for others, it is debilitating and causes disruption of daily life and routines.
Treatment can include painkillers for mild conditions or a minimally invasive surgical excision of Endometriosis.
Endometriosis excision is when the endometriotic lesions are removed surgically while preserving the uterus, fallopian tubes, and ovaries. This minimally invasive surgery is the most effective treatment for Endometriosis and should only be done by trained specialists.
People with severe deep infiltrating Endometriosis benefit highly from excision surgery. The improvement after this procedure for people with such cases is usually striking and highly successful.
Other treatments for Endometriosis include:
- Pelvic floor physiotherapy
- Pelvic floor Botox
- Change in diet
- Acupuncture
- Assessing and avoiding environmental triggers
Isthmocele or C-section scar defect or Uterine Niche
An isthmocele is an indentation or discontinuation in the uterine wall that results in the location of a Cesarean section scar. Its causes aren’t completely understood, but it is thought to be related to incomplete or abnormal healing of the uterine incision. This scar defect weakens and thins out the uterine wall at its location.
Isthmoceles can be asymptomatic but may produce symptoms and complications such as:
- Postmenstrual spotting,
- Painful periods,
- Painful intercourse
- Chronic pelvic pain
- Possible infertility
- Risk of uterine rupture or placental adhesion during pregnancy

Diagnosis
A uterine isthmocele can be detected incidentally on ultrasound or purposefully looked for by the physician if a patient is symptomatic.
The most accurate way to diagnose an isthmocele is with a saline infusion sonohysterogram (SIS). During this procedure, your gynecologist will inject a small amount of sterile saline into the uterine cavity through the vagina and visualize the lining using an ultrasound.
MRI is also used for the diagnosis of isthmocele.
Treatment
There are several ways in which a uterine niche could be treated ranging from expectant management and pharmacological treatment to surgery. Surgery could be done through open, minimally invasive, hysteroscopic and vaginal approaches. Hysteroscopy and laparoscopy are the most common approaches and desire for future fertility plays an important role in choosing a treatment modality.
- Hysteroscopy: Your doctor would shave or cauterize the defect from the inside. This works best for women with abnormal bleeding, a thick wall and no desire for future pregnancy.
- Laparoscopic repair: Your gynecologist would completely remove the defect and reconstruct the wall of the uterus. This option allows for a healthy future pregnancy as it removes the frail part of the muscle.
Adenomyosis is when tissue that lines your uterus grows into the muscular walls of your uterus.
It is ‘the presence of endometrial glands and stroma within the uterus or myometrium muscle. During monthly menstruation, this embedded tissue bleeds, leading to intense pelvic pain, inflammation and swelling, and heavy bleeding.
This condition is often misunderstood or misdiagnosed as Adenomyosis, often called Endometriosis of the uterus muscle, which causes both painful and heavy periods, painful sex, or dyspareunia.
With Endometriosis, spots of endometrial lining are located outside of the uterus, while in the case of Adenomyosis, this tissue is inside the muscle of the uterus… or an “Inside-Out Endometriosis”, as it used to be known.
To date, Adenomyosis has no clear causes, which can be frustrating. Studies have shown that people who have given multiple births and already suffer from Endometriosis are more at risk for Adenomyosis.
To diagnose Adenomyosis, a doctor will examine you and assess your symptoms. With this condition, the uterus may feel big, soft, tender, and sensitive to the touch.
Tests that your doctor can perform are:
- Ultrasound
- MRI
- Pathology examination after a Hysterectomy procedure.
As far as treatment goes, the symptoms of Adenomyosis can be dealt with by taking pain medication or by preventing monthly menstruation with hormonal treatment:
- Pain medication: The pain associated with Adenomyosis can be debilitating. Analgesics, anti-inflammatories, or strong painkillers can be prescribed.
- Hormonal Treatment: This is not a cure, as the pain will return if the treatment is stopped. Oral contraceptive pills, contraceptive implants (hormonal IUD), or injections can be suggested by your doctor to relieve pain and stop monthly periods.
- Surgery: If Adenomyosis is localized, it could be surgically excised. Sometimes the only solution to Adenomyosis is to remove the entire uterus. This procedure is called a Hysterectomy and may be suggested by your doctor based on your medical history, the extent of pain, and other symptoms.
Ovarian Cysts are growths developing within the ovaries
Most Ovarian Cysts are harmless and are not cancerous. Cysts on the ovaries can sometimes grow as big as a watermelon, whereas a normal ovary is around the size of an almond.
Ovarian Cysts are most common before Menopause, occurring in around 7% of women.
Although Ovarian Cysts are not necessarily harmful or cancerous, they should be taken seriously, because they could indicate other underlying conditions. Identifying and examining Ovarian Cysts is necessary to rule out cancer and any underlying causes, such as Endometriosis.
Ovarian Cysts can come in many different forms, each with a different cause:
- Functional cyst: These cysts form because of normal function of the ovaries. When ovulation does not happen and a follicular cyst remains in the ovaries, and the opening where the egg escapes is closed off with accumulated fluid.
- Pathological cyst: These cysts form because of disease, but are not necessarily cancerous.
- Dermoid cysts: These cysts grow with the existence of developmental tissue that can contain teeth, bone, or hair.
- Hemorrhagic cysts: These cysts form due to bleeding.
- Endometriomas: These cysts are caused by Endometriosis, and are a sign of a severe form of the condition, accompanied with a lot of pain.
- Cancerous cysts: These cysts are rare, but commonly affect post-menopausal people, with vague symptoms that can go undiagnosed.
With Ovarian Cysts, most symptoms are not always noticeable. With Endometriomas, however, the main symptom is severe pain, even when the cysts are small.
If the cysts are large, regardless of their type, symptoms can include pain and swelling in the abdominal area. Cysts can also lead to constipation or frequent urination due to the cysts pressing on other organs in the abdomen.
Complications of Ovarian Cysts can include twisting of the ovary, bleeding, or bursting of cysts, which can cause severe pain and bleeding, usually requiring emergency attention and treatment.
Diagnosing Ovarian Cysts can be done by assessing medical history and by examination. These tests include:
- Ultrasound
- Blood tests
- MRI
- CT scan
Your doctor should monitor some cysts, while others don’t need monitoring at all. Functional Cysts may go away on their own without being treated.
Some cysts require surgery, and this should be determined by your doctor, depending on the Condition
AUB, Abnormal Uterine Bleeding
AUB, Abnormal Uterine Bleeding, sometimes referred to as Abnormal Vaginal Bleeding, is a term used to refer to heavy periods or bleeding between normal periods. It is a common condition affecting around 10% to 20% of women in the US.
Menorrhagia, also known as heavy periods, occurs when excessive blood is lost during monthly menstrual cycles.
Metrorrhagia, also known as bleeding between periods, occurs when uterine bleeding occurs between menstruations.
AUB is not just uncomfortable and inconvenient, but it can also affect the person’s quality of life, whether physical, mental, or emotional.
This condition is not always associated with physical abnormalities. Approximately 40% to 60% of people with heavy periods have no specific underlying cause.
AUB is associated with:
- Leaking through sanitary pads
- The necessity for double protection
- Flooding of menstrual blood onto clothes
- Large clots in the blood
- Sensations of weakness, tiredness
- Anemia
- Planning daily life around menstruation
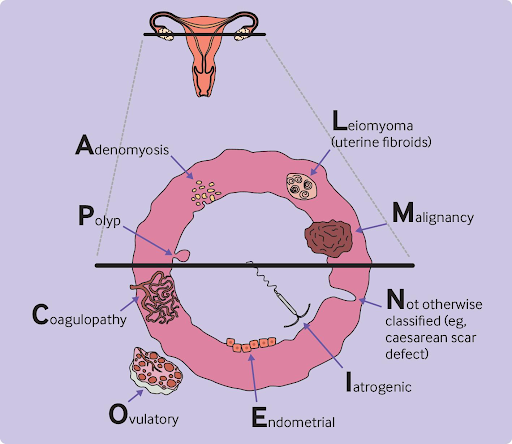
Although the majority of people with AUB have no specific underlying cause, there are some known reasons :
- Polyps: non-cancerous growths in the lining of the uterus
- Endometriosis: when developed in the vagina and/or the lower uterus
- Fibroids: benign growths on the walls of the uterus
- Adenomyosis: when glands from the uterus lining embed in the muscle of the uterus
- Cancer: uterine cancer is uncommon but can cause heavy periods
- Thyroid disease: thyroid disease can cause tiredness, weight gain, changes in hair and skin, intolerance to colds, and AUB
- Clotting problems: platelet problems or certain diseases can affect clotting and increase AUB
- Medical treatments: some medical treatments, such as hormonal contraceptives, anticoagulants, and anti-cancer drugs, can cause AUB
- Blood tests,
- Ultrasound
- Hysteroscopy (a camera to visualize the cavity of the uterus)
As for treatments, there are many options available, including:
- Hormonal and non-hormonal treatments
- Endometrial ablation
- Minimally invasive surgical removal of fibroids and polyps
- Hysterectomy
Tubo-ovarian abscess
A tubo-ovarian abscess (TOA) is an infectious mass found in the fallopian tube, ovary, or near those structures. It can be due to several factors that introduce an infection, but it usually develops as a pelvic inflammatory disease (PID) complication. PID is an infection of the pelvic reproductive organs that results mainly from untreated sexually transmitted infections.
Bacteria can travel up the vagina into the uterus, reaching the tubes and ovaries to form a walled-off cyst known as a tubo-ovarian abscess. TOAs occur in around 15% of patients with PID and are usually polymicrobial, meaning several types of bacteria are isolated from the abscess.
A TOA can be life-threatening should it rupture and cause sepsis, a widespread infection in the patient’s bloodstream.
Risk factors for developing a TOA include:
- Young age
- Multiple sexual partners
- Sexually transmitted infections
- Uterine instrumentation, such as insertion of an IUD with an active infection or a dilation and curettage (D&C)
- Hysteroscopy

Symptoms
- Lower abdominal pain
- Fever and/or chills
- Vaginal discharge
- Painful intercourse
- Nausea & vomiting
Evaluation & Diagnosis
On suspicion of a tubo-ovarian abscess, your doctor will perform a transvaginal ultrasound and may be able to identify the mass. Further imaging, usually a CT scan, might be needed to visualize the abscess better.
Although not commonly used, laparoscopy is still considered the definitive diagnostic tool and may allow for drainage and culture of the abscess.
Treatment
The first step in managing a TOA is starting antibiotics to avoid a widespread infection. Imaging-guided drainage by a radiologist could be attempted during antibiotic treatment.
While on this regimen, patients should be monitored for worsening symptoms or lack of improvement, which would then require surgical intervention to remove the abscess along with the affected tube or ovary.
Complications
- Recurrent PIDs
- Chronic pelvic pain
- Ectopic pregnancy, outside of the uterus
- Infertility

