Procedures
RPSA, the Center for Endoscopic and Advanced Procedures, is known for its remarkable and efficient medical services. With a team of highly skilled professionals and state-of-the-art facilities, RPSA specializes in a variety of medical procedures that cater to their patient’s convenience and comfort. Amongst the numerous procedures offered, the most commonly performed ones include minimally invasive approaches, which are recommended and carried out by Dr. Iskander himself. Regarded as a pioneer in this field, Dr. Iskander firmly believes that no condition is too complex for minimally invasive surgery. He has spent years training, advocating, and speaking about such techniques, which not only provide quicker recovery times for the patient but also reduce the risk of complications that a more invasive surgery can bring with it. With RPSA, you can be sure of receiving the best medical care possible, making your road to recovery a smooth and comfortable one.
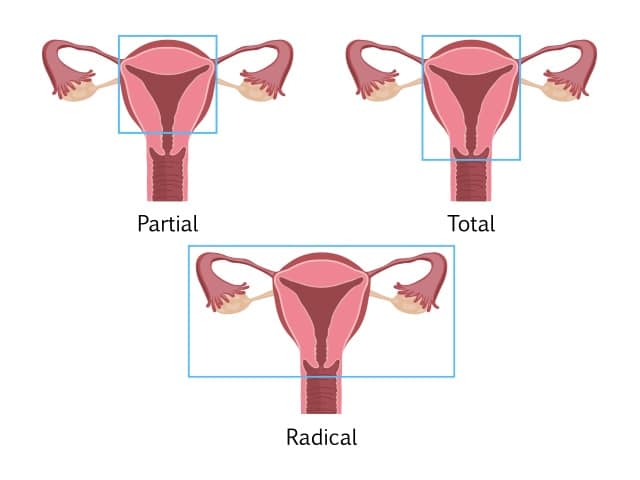
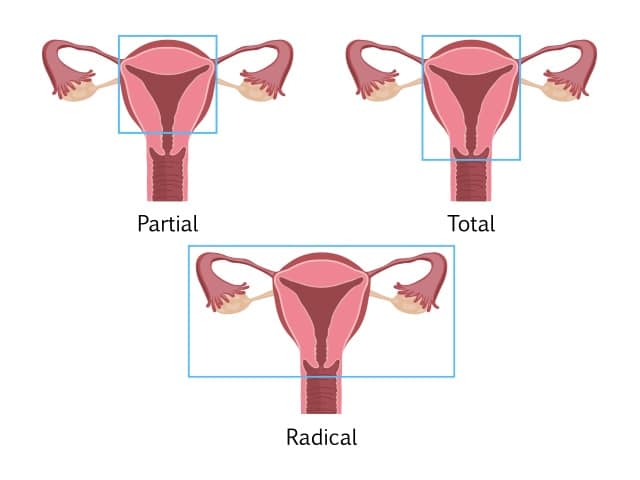
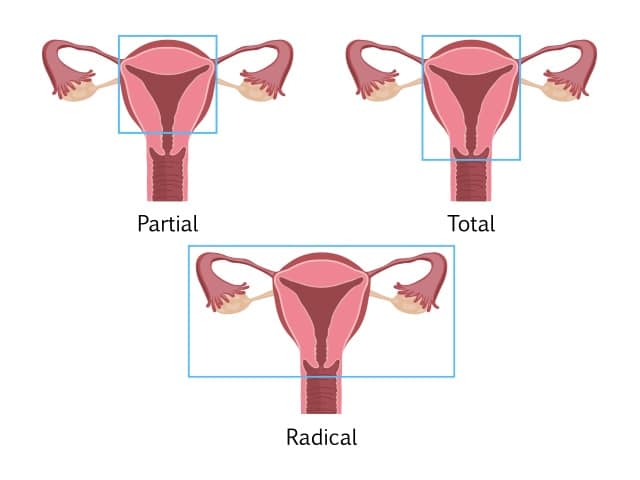
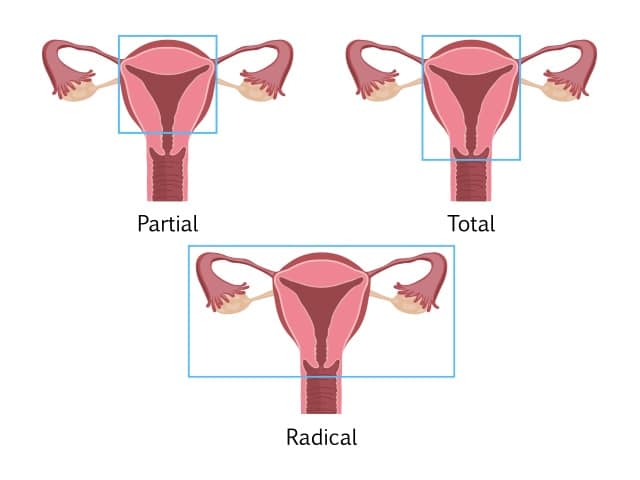
A Hysterectomy is a gynecological procedure that usually entails removing the entire uterus, including the cervix.
There are different types of hysterectomies: Supracervical Hysterectomy, which entails removing the uterus while leaving the cervix in place, and Total Hysterectomy, which entails removing the uterus along with the cervix.
The term Hysterectomy, whether total or supracervical, is only specific to surgery on the uterus and does not include removal of the ovaries.
Removing the ovaries and the uterus is not recommended in patients under 65 years old unless indicated by your doctor. Removing the ovaries with a Hysterectomy is referred to as Oopherectomy.
It is also recommended at the time of Hysterectomy to remove the fallopian tubes. Studies have shown that removing the fallopian tubes during a Hysterectomy can decrease the risk of future cancer of the ovaries and fallopian tubes by 30%.
Hysterectomies are performed to relieve the following conditions:
- Adenomyosis
- As part of pelvic prolapse repair
- Heavy bleeding, with or without Fibroids
- Pelvic pain with origin in the uterus
- Painful intercourse with origin in the uterus
At Reston OBGYN, our preferred method of performing Hysterectomies is through a minimally invasive approach that could be done successfully in almost all cases, irrelevant of the size of the uterus or the complexity of the procedure.
This technique carries lower risks of complications and requires only small incisions, resulting in quicker recovery.
This procedure is ideal as it gives full access to the pelvis, allowing the doctor to evaluate and treat potentially associated conditions, such as endometriosis, scar tissue, and ovarian cysts.
After a Hysterectomy, people can be discharged the same day and return to their full, normal activity in around two weeks (aside from sex).
Sexual intercourse should only be resumed after at least eight weeks and if you feel comfortable.
You might experience the following after a Hysterectomy:
- General pain that should resolve with time
- Pain around the incisions that should last only a few days
- Pelvic and rectal pain and pressure should resolve with time
- Chest and shoulder pain that should resolve within 2 to 3 days
- Bruises at the incisions that will resolve on their own
- Vaginal spotting during the first week
- Nausea caused by anesthesia and pain medication
- Swelling of the abdomen that will resolve over time
- Constipation due to medication
- Diarrhea caused by antibiotics
- Urinary retention due to anesthetics (seek your doctor’s advice if this occurs after you are sent home)
As part of your recovery, you might be given prescription medication to ease the the pain. It is important not to drive when taking any prescribed narcotics. Avoid lifting, swimming, and heavy exercise. Use caution when starting an exercise routine after your procedure, starting slowly and listening to your body to ensure you are comfortable and able.
A Hysterectomy will cause periods to stop. However, hormone production should not be affected if ovaries are spared during the surgery. After a hysterectomy, you cannot conceive, so this procedure is not recommended for people desiring fertility or childbearing.
A Hysterectomy will not cause early menopause unless both ovaries have been removed during the procedure. In this case, Estrogen replacement therapy can prevent menopausal symptoms, such as hot flashes, vaginal dryness, and night sweats. You can discuss this with your doctor based on the procedure you undergo and what is best for your body.
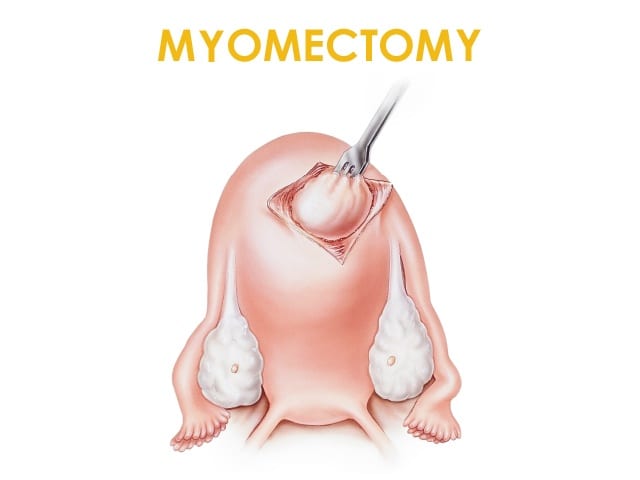
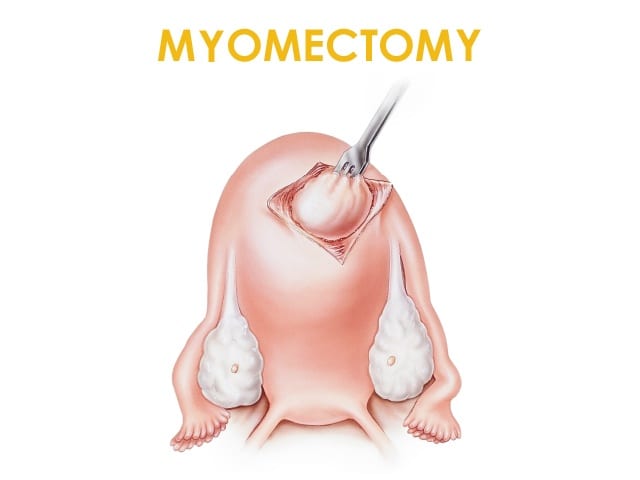
A Myomectomy is a surgical procedure to remove Fibroids while keeping the uterus in place.
Fibroids can lead to abnormal uterine bleeding, difficulty conceiving, miscarriages, large and bulky uterus, and other serious complications during pregnancy.
A Myomectomy is suggested for people with fibroids who still wish to maintain their fertility.
This procedure is rarely performed on people who no longer wish to have children.
Your doctor, following examinations, and depending on the location of the fibroids and their type, will determine the type of Myomectomy you need.
Depending on the location of your fibroids and your symptoms, a hysteroscopic or a laparoscopic myomectomy could be offered by your surgeon.
Unfortunately, many patients are still offered a traditional Myomectomy, mainly due to the complexity of their case (large or multiple fibroids) and the inexperience of their surgeon.

Minimally invasive and robotic surgeries are always an option for patients at Reston OBGYN, even in the case of complex Myomectomies.
Recovering from a Myomectomy takes approximately two weeks, with patients returning to work and normal activity within 7 to 10 days.
Sex should be avoided for at least two weeks after the procedure and only resumed once you feel comfortable.
After your procedure, and depending on the technique used, you might experience the following:
- Bruises or scars at the incision sites
- Bleeding and spotting similar to menstruation a few days after surgery
- Swelling in arms and legs due to increase fluid intake during your procedure
- Swelling in abdominal area
- Constipation due do medication
- Diarrhea caused by antibiotics
- Urinary retention
- Pain around incision sites
- Pain in pelvic and rectal areas
- Chest and shoulder pain
- Nausea due to anesthesia and/or medication
It is important to be cautious about starting an exercise routine after surgery. Listen to your body and respects its limits.
After a Myomectomy, fertility will be retained, but it is important to allow the uterus to heal completely before trying to conceive. Be sure to consult your doctor about this.
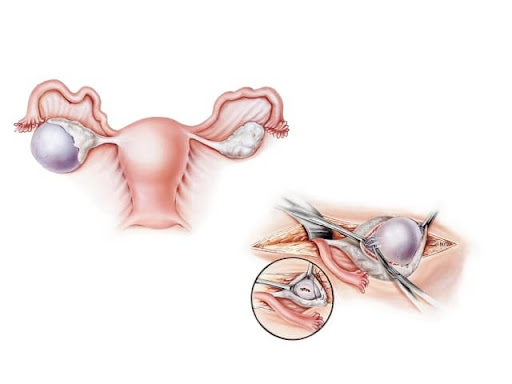
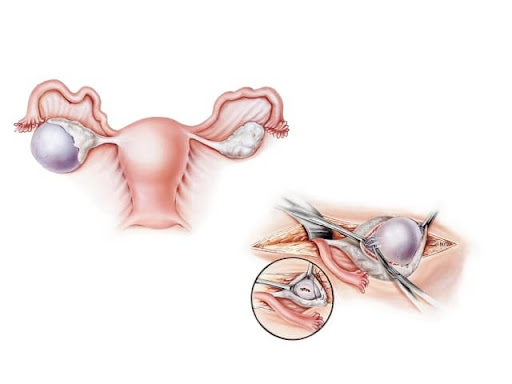
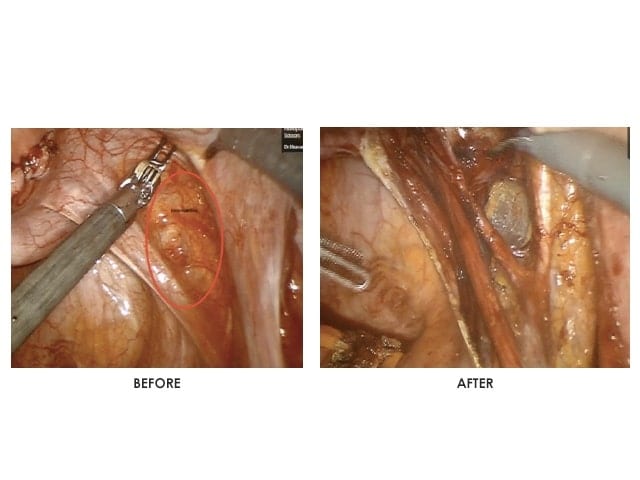
An Ovarian Cystectomy is the removal of ovarian cysts or tumors, while still preserving the ovaries.
Ovarian cysts are common, and your doctor can decide on the best treatment and procedure for you based on the size and the type of the cyst or tumor, your age, and possible malignancy.
An Ovarian Cystectomy is almost always done with a minimally invasive procedure that involves small skin incisions using laparoscopic or robotic techniques.
If a cyst is suspected to be malignant, full removal of the ovary might be necessary to avoid rupturing and spread of the cancerous cells into the pelvic area.
Removing the cyst from the ovary can affect your ovarian reserve. Discuss with your doctor the best approach.Ovarian cystectomy requires an experienced surgeon to minimize damage to healthy ovarian tissues during the procedure and minimize damage to the ovary.
Once the cyst is removed successfully, it is always sent for testing to rule out malignancy.
After a minimally invasive procedure, recovery is quick, and pain is usually minimal. This procedure is an outpatient procedure, and patients are up walking within hours.
Patients can usually go back to normal activity and work within 1-2 weeks.
To relieve pain, your doctor may prescribe you medication.
An oophorectomy is a surgical procedure during which one or both of your ovaries are removed.
Why would you remove your ovaries?
There are several reasons for which you might need an oophorectomy. Below are the most common ones:
- A tubo-ovarian abscess, which is a pus-filled sac involving your fallopian tube and ovary. This is usually the result of an untreated infection. An abscess usually presents with fever and pelvic pain.
- Ovarian cancer: oophorectomy can be either therapeutic to remove the tumor or prophylactic to prevent the development of a cancer if you are known to have a genetic predisposition.
- Ovarian endometriosis or other benign cysts which might cause pelvic pain, period irregularities, ovarian torsion, and infertility. Removal of the pathology can help relieve symptoms. For benign conditions like endometriosis and cysts, the removal of an ovary should be the last resort to treat these pathologies, and an ovarian sparing approach should be always attempted.
- Ectopic pregnancy, which is a pregnancy that implants in the tube or on the ovary. Ectopic pregnancies are not viable, and if the sac and embryo get too big for medical treatment, you might need to have them removed surgically.
Oophorectomy can be unilateral if fertility is still desired or bilateral if fertility is no longer desired or if medically indicated. The removal of the ovary is sometimes accompanied by the removal of the fallopian tube as well, depending on the extent of pathology, and this procedure is termed salpingo-oophorectomy.
Your gynecologist will offer you the type of surgery that best treats your condition while considering your desire for future fertility.
Like other surgeries, oophorectomy can be done via laparoscopy or a robot and remain minimally invasive instead of an open approach that leaves the patient with a big scar and higher rates of complications.
A minimally invasive procedure will allow you to leave the hospital within a day ofthe operation. Laparoscopy and robot-assisted surgery also speed up recovery and get you back to regular activity within two weeks.
At RPSA, we always opt for minimally invasive approaches to provide the best experience for our patients with the least side effects and complications. Ovarian sparing surgery is always the first-line therapy for benign ovarian pathology.
Dr. Iskander is a highly reputable leading expert in this domain.
What to expect after an oophorectomy?
If you have gotten a bilateral oophorectomy, you may experience symptoms of menopause such as:
- Hot flashes
- Vaginal dryness
- Depression
- Decreased sex drive
Your doctor might start you on hormonal or non-hormonal medications to accustom your body to these changes and decrease the unpleasant symptoms that you might experience.
Why would you remove your ovaries?
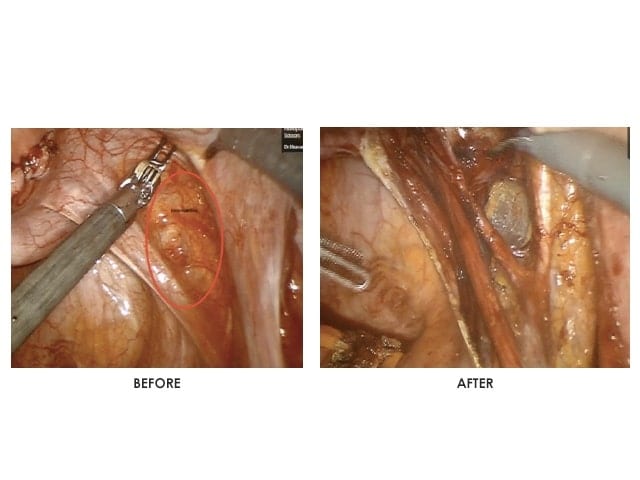
Endometriosis Excision is a procedure that removes Endometriotic lesions that could be located in the pelvis or outside the pelvis, depending on your case. Removing all endometriotic lesions is essential to relieving the pain caused by this disease.
This procedure is minimally invasive through Laparoscopy or Robotic Surgery, and allows for managing pain and infertility associated with Endometriosis. It is the gold standard to manage this condition.
Endometriosis excision requires advanced surgical skills and well trained surgeons, especially in cases of deeply infiltrating endometriosis, where the surgical anatomy is challenging for inexperienced surgeons.
Endometriosis Excision, through only a few small skin incisions, using a thin camera that is inserted into the pelvic area, allows the endometriotic lesions to be cut out and removed.
Endometriosis treatment requires a comprehensive management plan set up with your doctor. Excision followed by appropriate management could help reduce the risk of recurrence of the disease.
- Pain that should resolve daily
- Pain around site of incisions
- Chest and shoulder pain
- Vaginal spotting
- Nausea caused by anesthesia or pain medication
- Swelling of arms and legs due to fluid retention
- Swelling of the abdomen due to irritation of intestines
- Constipation
- Diarrhea caused by antibiotics
- Urinary retention
- Bruises or scars around the incision areas
A Hysterectomy is a gynecological procedure that usually entails removing the entire uterus, including the cervix.
There are different types of hysterectomies: Supracervical Hysterectomy, which entails removing the uterus while leaving the cervix in place, and Total Hysterectomy, which entails removing the uterus along with the cervix.
The term Hysterectomy, whether total or supracervical, is only specific to surgery on the uterus and does not include removal of the ovaries.
Removing the ovaries and the uterus is not recommended in patients under 65 years old unless indicated by your doctor. Removing the ovaries with a Hysterectomy is referred to as Oopherectomy.
It is also recommended at the time of Hysterectomy to remove the fallopian tubes. Studies have shown that removing the fallopian tubes during a Hysterectomy can decrease the risk of future cancer of the ovaries and fallopian tubes by 30%.
Hysterectomies are performed to relieve the following conditions:
- Adenomyosis
- As part of pelvic prolapse repair
- Heavy bleeding, with or without Fibroids
- Pelvic pain with origin in the uterus
- Painful intercourse with origin in the uterus
At Reston OBGYN, our preferred method of performing Hysterectomies is through a minimally invasive approach that could be done successfully in almost all cases, irrelevant of the size of the uterus or the complexity of the procedure.
This technique carries lower risks of complications and requires only small incisions, resulting in quicker recovery.
This procedure is ideal as it gives full access to the pelvis, allowing the doctor to evaluate and treat potentially associated conditions, such as endometriosis, scar tissue, and ovarian cysts.
After a Hysterectomy, people can be discharged the same day and return to their full, normal activity in around two weeks (aside from sex).
Sexual intercourse should only be resumed after at least eight weeks and if you feel comfortable.
You might experience the following after a Hysterectomy:
- General pain that should resolve with time
- Pain around the incisions that should last only a few days
- Pelvic and rectal pain and pressure should resolve with time
- Chest and shoulder pain that should resolve within 2 to 3 days
- Bruises at the incisions that will resolve on their own
- Vaginal spotting during the first week
- Nausea caused by anesthesia and pain medication
- Swelling of the abdomen that will resolve over time
- Constipation due to medication
- Diarrhea caused by antibiotics
- Urinary retention due to anesthetics (seek your doctor’s advice if this occurs after you are sent home)
As part of your recovery, you might be given prescription medication to ease the the pain. It is important not to drive when taking any prescribed narcotics. Avoid lifting, swimming, and heavy exercise. Use caution when starting an exercise routine after your procedure, starting slowly and listening to your body to ensure you are comfortable and able.
A Hysterectomy will cause periods to stop. However, hormone production should not be affected if ovaries are spared during the surgery. After a hysterectomy, you cannot conceive, so this procedure is not recommended for people desiring fertility or childbearing.
A Hysterectomy will not cause early menopause unless both ovaries have been removed during the procedure. In this case, Estrogen replacement therapy can prevent menopausal symptoms, such as hot flashes, vaginal dryness, and night sweats. You can discuss this with your doctor based on the procedure you undergo and what is best for your body.
A Myomectomy is a surgical procedure to remove Fibroids while keeping the uterus in place.
Fibroids can lead to abnormal uterine bleeding, difficulty conceiving, miscarriages, large and bulky uterus, and other serious complications during pregnancy.
A Myomectomy is suggested for people with fibroids who still wish to maintain their fertility.
This procedure is rarely performed on people who no longer wish to have children.
Your doctor, following examinations, and depending on the location of the fibroids and their type, will determine the type of Myomectomy you need.
Depending on the location of your fibroids and your symptoms, a hysteroscopic or a laparoscopic myomectomy could be offered by your surgeon.
Unfortunately, many patients are still offered a traditional Myomectomy, mainly due to the complexity of their case (large or multiple fibroids) and the inexperience of their surgeon.

Minimally invasive and robotic surgeries are always an option for patients at Reston OBGYN, even in the case of complex Myomectomies.
Recovering from a Myomectomy takes approximately two weeks, with patients returning to work and normal activity within 7 to 10 days.
Sex should be avoided for at least two weeks after the procedure and only resumed once you feel comfortable.
After your procedure, and depending on the technique used, you might experience the following:
- Bruises or scars at the incision sites
- Bleeding and spotting similar to menstruation a few days after surgery
- Swelling in arms and legs due to increase fluid intake during your procedure
- Swelling in abdominal area
- Constipation due do medication
- Diarrhea caused by antibiotics
- Urinary retention
- Pain around incision sites
- Pain in pelvic and rectal areas
- Chest and shoulder pain
- Nausea due to anesthesia and/or medication
It is important to be cautious about starting an exercise routine after surgery. Listen to your body and respects its limits.
After a Myomectomy, fertility will be retained, but it is important to allow the uterus to heal completely before trying to conceive. Be sure to consult your doctor about this.
An Ovarian Cystectomy is the removal of ovarian cysts or tumors, while still preserving the ovaries.
Ovarian cysts are common, and your doctor can decide on the best treatment and procedure for you based on the size and the type of the cyst or tumor, your age, and possible malignancy.
An Ovarian Cystectomy is almost always done with a minimally invasive procedure that involves small skin incisions using laparoscopic or robotic techniques.
If a cyst is suspected to be malignant, full removal of the ovary might be necessary to avoid rupturing and spread of the cancerous cells into the pelvic area.
Removing the cyst from the ovary can affect your ovarian reserve. Discuss with your doctor the best approach.Ovarian cystectomy requires an experienced surgeon to minimize damage to healthy ovarian tissues during the procedure and minimize damage to the ovary.
Once the cyst is removed successfully, it is always sent for testing to rule out malignancy.
After a minimally invasive procedure, recovery is quick, and pain is usually minimal. This procedure is an outpatient procedure, and patients are up walking within hours.
Patients can usually go back to normal activity and work within 1-2 weeks.
To relieve pain, your doctor may prescribe you medication.
An oophorectomy is a surgical procedure during which one or both of your ovaries are removed.
Why would you remove your ovaries?
There are several reasons for which you might need an oophorectomy. Below are the most common ones:
- A tubo-ovarian abscess, which is a pus-filled sac involving your fallopian tube and ovary. This is usually the result of an untreated infection. An abscess usually presents with fever and pelvic pain.
- Ovarian cancer: oophorectomy can be either therapeutic to remove the tumor or prophylactic to prevent the development of a cancer if you are known to have a genetic predisposition.
- Ovarian endometriosis or other benign cysts which might cause pelvic pain, period irregularities, ovarian torsion, and infertility. Removal of the pathology can help relieve symptoms. For benign conditions like endometriosis and cysts, the removal of an ovary should be the last resort to treat these pathologies, and an ovarian sparing approach should be always attempted.
- Ectopic pregnancy, which is a pregnancy that implants in the tube or on the ovary. Ectopic pregnancies are not viable, and if the sac and embryo get too big for medical treatment, you might need to have them removed surgically.
Oophorectomy can be unilateral if fertility is still desired or bilateral if fertility is no longer desired or if medically indicated. The removal of the ovary is sometimes accompanied by the removal of the fallopian tube as well, depending on the extent of pathology, and this procedure is termed salpingo-oophorectomy.
Your gynecologist will offer you the type of surgery that best treats your condition while considering your desire for future fertility.
Like other surgeries, oophorectomy can be done via laparoscopy or a robot and remain minimally invasive instead of an open approach that leaves the patient with a big scar and higher rates of complications.
A minimally invasive procedure will allow you to leave the hospital within a day ofthe operation. Laparoscopy and robot-assisted surgery also speed up recovery and get you back to regular activity within two weeks.
At RPSA, we always opt for minimally invasive approaches to provide the best experience for our patients with the least side effects and complications. Ovarian sparing surgery is always the first-line therapy for benign ovarian pathology.
Dr. Iskander is a highly reputable leading expert in this domain.
What to expect after an oophorectomy?
If you have gotten a bilateral oophorectomy, you may experience symptoms of menopause such as:
- Hot flashes
- Vaginal dryness
- Depression
- Decreased sex drive
Your doctor might start you on hormonal or non-hormonal medications to accustom your body to these changes and decrease the unpleasant symptoms that you might experience.
Why would you remove your ovaries?
Endometriosis Excision is a procedure that removes Endometriotic lesions that could be located in the pelvis or outside the pelvis, depending on your case. Removing all endometriotic lesions is essential to relieving the pain caused by this disease.
This procedure is minimally invasive through Laparoscopy or Robotic Surgery, and allows for managing pain and infertility associated with Endometriosis. It is the gold standard to manage this condition.
Endometriosis excision requires advanced surgical skills and well trained surgeons, especially in cases of deeply infiltrating endometriosis, where the surgical anatomy is challenging for inexperienced surgeons.
Endometriosis Excision, through only a few small skin incisions, using a thin camera that is inserted into the pelvic area, allows the endometriotic lesions to be cut out and removed.
Endometriosis treatment requires a comprehensive management plan set up with your doctor. Excision followed by appropriate management could help reduce the risk of recurrence of the disease.
- Pain that should resolve daily
- Pain around site of incisions
- Chest and shoulder pain
- Vaginal spotting
- Nausea caused by anesthesia or pain medication
- Swelling of arms and legs due to fluid retention
- Swelling of the abdomen due to irritation of intestines
- Constipation
- Diarrhea caused by antibiotics
- Urinary retention
- Bruises or scars around the incision areas

